The heart is more than just a muscle. A complex electrical system drives the heart’s chambers to contract in a coordinated rhythm, pushing blood out to every cell in the body. When the system is damaged by heart disease, short circuits can result, causing dangerous disturbances in heart rhythm called arrhythmias.
It is estimated that by 2050, 5 million to 10 million people in North America will have atrial fibrillation, the most common form of arrhythmia. As more and more people survive heart attacks and live longer with chronic heart disease, they can be left with scarred and damaged heart tissue that contributes to arrhythmias, some of which are potentially fatal.
Implantable devices to regulate and synchronize the heartbeat, catheter-based ablation procedures to cauterize locations in the heart that cause irregular electrical signals, and drugs that help to control abnormal heart rhythms are all becoming more and more central to cardiology.
The Electrophysiology Toolbox
Electrophysiologists have a growing range of options for treating heart rhythm disorders, from long-used medications to cutting-edge, catheter-based procedures.
Medications: Medication is usually the first option. Anti-arrhythmics can be used to control certain arrhythmias that cause discomfort to patients. But because these drugs can have serious side effects—and do not always provide relief—they are not appropriate for all patients. Other medications, such as beta blockers, may also be used to treat arrhythmias. In situations where medication is not the solution, electrophysiologists look next to device implantation or ablation.
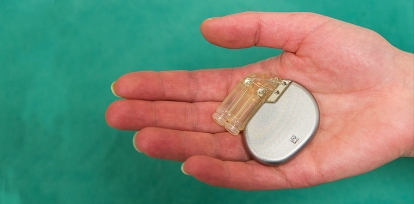
Implantable Devices: The devices used regularly by electrophysiologists are pacemakers, implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy (CRT) devices.
- Familiar to many people, a pacemaker is a small device (about the size of a pager) that is placed surgically under a patient’s skin near the heart. It continuously monitors the electrical activity of the heart and temporarily takes control of the heartbeat when it becomes abnormal.
- An ICD is a device that, like a pacemaker, continuously monitors the heartbeat but can also deliver an electrical shock to restore normal heart rhythm when needed. The Heart Institute EP group recently implanted an experimental subcutaneous defibrillator that has no wires touching the heart.
- A CRT device stimulates and coordinates the pumping chambers of the heart. It can be implanted as part of a pacemaker or an ICD system.
Ablation: To ablate means to destroy, but cardiac ablations are tightly controlled procedures that target only the small areas of heart tissue that generate abnormal electrical signals. After painstakingly mapping the electrical patterns in a patient’s heart, tiny probes, placed on the ends of catheters, are threaded through veins to the affected chambers of the heart where they are used to kill off abnormal tissue, most often using high-frequency radio waves.
Before the development of catheter-based techniques, cardiac ablation required highly invasive open heart surgery. Today, ablations can be safely performed in many patients who could not tolerate a surgical procedure, and recovery times are much shorter.
This is the world of electrophysiology (EP). Just as blocked or damaged blood vessels and valves can be repaired without surgery by interventional cardiologists, interventional electrophysiologists fix the heart’s circuitry. “We joke that they’re the plumbers and we’re the electricians,” said Dr. David Birnie, an electrophysiologist and Director of the Arrhythmia Service at the University of Ottawa Heart Institute.
They are looking for ways to detect arrhythmias early and to prevent them from becoming persistent and symptomatic.
EP is a relatively young specialty. The Arrhythmia Service was started in 1983 by Dr. Martin Green, who had received training in the new discipline from one of its founders, in Maastricht, the Netherlands. Today the Heart Institute has eight full-time electrophysiologists, bringing together training and expertise from four continents.
“It’s a rapidly evolving field,” said Dr. Calum Redpath, an electrophysiologist and clinician-scientist who joined the Heart Institute in 2010. “In 1983, accurate diagnosis of arrhythmia was just emerging, but then people had to be told ‘You’ve got this arrhythmia, but there’s nothing much we can do about it.’ Now, for the vast majority of patients with arrhythmias, we can cure them with ablation. And for the ones that we can’t, we’re working very hard to see if we can improve the ablation procedures so that they’re curative.”
A GPS System for the Heart
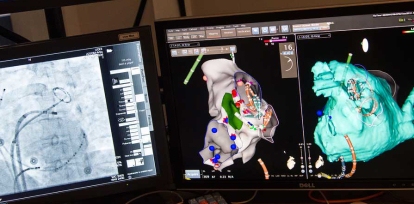
A huge leap forward for the field came in the late 1990s, with the development of sophisticated electrical mapping systems, explained Dr. Pablo Nery, another member of the EP team. This technology allows physicians to pinpoint the areas of the heart that generate abnormal electrical signals and then precisely destroy the disruptive tissue using high-frequency radio waves. This destruction—called ablation—targets only the specific, small areas that cause abnormal electrical activity and spares normal heart tissue.
Using a special operating table that generates a magnetic field around the patient, the doctor inserts a catheter with a smaller sensor into a vein. This is fed into the chamber of the heart that is generating the arrhythmia and then methodically placed in contact with specific regions of heart tissue in that chamber. The electrical signals detected by the catheter are picked up by the table’s larger magnetic field and turned into a detailed 3-D map of each chamber’s electrical activity—both normal and abnormal.
“With normal heart muscle, we get normal signals and higher voltage. When we have the catheter in contact with scar tissue, for example, an abnormal reading is recorded. This allows us to create an electrical map of the heart and know exactly which areas may be involved in the arrhythmia. This technology allows the physician to identify these critical areas and to go back precisely to a region, if necessary, which was not possible in the past,” explained Dr. Nery.
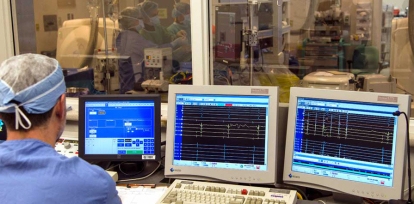
The new systems make it possible for nearly all patients to undergo diagnostic mapping and ablation treatment in the same sitting. However, complex ablations are long, involved procedures, explained Dr. Robert Lemery, who trained in the Netherlands early in his career and came to the Heart Institute 10 years ago. They require not only the lead electrophysiologist and an anesthesiologist but an assisting doctor, a nurse and two technicians to handle the software in real time.
One technician oversees the continuous electrical readout. When the doctor needs to look at a particular location in the heart in more detail, a good deal of back-and-forth communication is necessary as the technician and doctor work to identify abnormal areas.
A second technician annotates the 3-D map of the heart throughout the procedure to provide a record of what has been done: which locations were tested and which were ablated. The entire process can be very time consuming. “Because we’re working at the tip of a catheter positioned inside the heart, it can take time to get back to a specific point of interest,” said Dr. Lemery.
And sometimes it’s a waiting game. “A patient may have an intermittent racing heartbeat. Five beats may go by and we can record it, and then we wait and wait for the heart to do the same thing again. Sometimes, we have to provoke it, but in some cases, it can take hours,” he added. Every person’s arrhythmia has a unique electrical cause, meaning that there can be no shortcuts. Each heart must be mapped and uniquely ablated.
A Growing Range of Tools and Techniques
Other recent advances in technology include improved catheters, in particular ones that hold a miniature echocardiography system to allow real-time imaging guidance to and through the heart. These, along with better ablative instruments, mainly using radio frequency, allow electrophysiologists to correct arrhythmias that were untreatable only a decade ago.

“In the 1990s, we used to do very simple cases, but we were not able to handle most of the cases we do today. We can now cover 80 or 90% of the conditions that we see,” said Dr. Girish Nair, who was recruited from McMaster University in the fall of 2012.
The Heart Institute team now performs a wide range of complex procedures available at only a few institutions in Canada. These include ablation for atrial fibrillation, in which catheters must be carefully passed through the septum—the barrier between the heart’s chambers—and ablation for ventricular tachycardia, which involves equally complex issues of access, often in very sick patients.
Sometimes ventricular tachycardia is caused by abnormal tissue on the outside of the heart, explained Dr. Pablo Nery, another member of the EP team. This requires an approach called epicardial ablation, in which a needle is inserted through the chest wall and used to guide a catheter into the membrane protecting the heart in order to bring it directly in contact with the heart’s exterior. In the past, reaching this abnormal tissue would have required open heart surgery. “Now we can use catheters, avoiding an extensive procedure and allowing patients to recover faster, with equivalent outcomes.”
A specialty Dr. Nair brought to the Heart Institute is ablation for adolescent and teenage patients, who very few electrophysiologists in Canada can treat because they have complex arrhythmias caused by either genetic conditions or congenital abnormalities.
Having many options for different conditions all within the Heart Institute is important, explained Dr. Nair, because not all patients with a certain type of arrhythmia are alike, and different patients may require very different approaches for treating their conditions. “Ultimately, we don’t want to have to send any patient away to another centre for a procedure,” said Dr. Birnie.

Research to Prevent and Treat Arrhythmias
Although pacemakers have been available for around 50 years, the first implantable cardioverter defibrillator (ICD) was only implanted in 1985. (See “The Electrophysiology Toolbox” sidebar for more information on EP treatment options.)
The first cardiac resynchronization therapy (CRT) device was placed in a patient in 1994. A major international clinical trial led by the Heart Institute, called RAFT, showed in 2010 that CRT can reduce the risk of death for patients with symptoms of mild to moderate heart failure. The finding changed clinical practice worldwide and was recognized as landmark research.
Catheter-based ablative techniques were first used in humans in the late 1980s, and the first catheter procedure to ablate atrial fibrillation, the most common type of arrhythmia, was performed in 1998.
Because EP is a rapidly evolving field, Heart Institute doctors are heavily involved in clinical research comparing new ablative procedures to older drug therapies and working out the best techniques for performing the procedures. Substantial progress has already been made in streamlining ablations. Procedures that would have taken five or six hours 10 years ago now take around three or four hours, said Dr. Nery.
The group is also looking for better ways to manage its growing volume of arrhythmia patients. “We’re working with our primary care colleagues in the community to develop ways to handle patients with arrhythmias more efficiently, to reduce waiting times and to give them the correct treatment based on the best evidence. That’s another form of innovation—streamlining care,” said Dr. Nair
But even the most optimized procedures and relationships with community practitioners will not be enough to stave off the upcoming wave of patients needing arrhythmia management, especially for atrial fibrillation. As Dr. Redpath explained, the demand for care is compounded by the fact that atrial fibrillation is often a chronic condition, requiring re-treatment as the disease progresses.
“It’s an epidemic, and it’s going to completely explode over the next 25 years,” he said. “We can’t ablate that many people—it’s just not sustainable. For those patients who have atrial fibrillation now, it’s a brilliant treatment, but it’s not the answer to the problem. The answer is either to prevent it, or if we can’t, to delay it.”
Common Arrhythmias
An arrhythmia is a disorder that affects the heart rate and rhythm. Although many arrhythmias rarely cause serious health problems, some can be rapidly fatal and require expert diagnosis and management.
Some of the most common arrhythmias that require treatment are:
- Atrial fibrillation: an irregular rhythm in the heart’s upper chambers. Atrial fibrillation is the most common type of arrhythmia and can lead to uncomfortable symptoms, heart failure and stroke. About one-third of all strokes are caused by atrial fibrillation.
- Ventricular tachycardia: a very rapid heart rate that begins in the ventricles, the heart’s lower chambers. Ventricular tachycardia can cause loss of consciousness and sudden cardiac death when blood cannot be pumped out of the heart.
- Supraventricular tachycardia: a rapid heart rate that begins around the electrical connection point between the upper and lower chambers of the heart, called the atrioventricular node. Though not as dangerous as ventricular tachycardia, supraventricular tachycardia can cause distressing symptoms, including difficulty breathing, chest pain and loss of consciousness.
- Bradycardia: an abnormally slow heart rate, which can cause difficulty in breathing, loss of consciousness or death in rare cases if the heart rate drops too low.
Dr. Redpath and the team’s two other clinician-scientists, Dr. Michael Gollob and Dr. Darryl Davis, devote their time to more basic research in addition to clinical care and research. They are looking for ways to detect arrhythmias early and to prevent them from becoming persistent and symptomatic. Dr. Gollob, Director of the Inherited Arrhythmia Clinic, specializes in understanding the genetic risk factors for arrhythmias, which may someday help with early detection. Dr. Davis focuses on regenerative medicine, working to harness the body’s own stem cells to repair scar tissue in the heart before it can alter the electrical system.
Dr. Redpath is trying to understand the cellular mechanisms that allow what starts out as intermittent electrical abnormalities to change the heart tissue over time, so that the heart actually “prefers” an arrhythmia to normal signalling, a process called remodelling. He hopes to understand this process at the cellular level, and then interrupt it.
“I’m also trying to establish smarter ways of picking up atrial fibrillation earlier so you don’t have to wait until patients are symptomatic or unwell, or have a stroke,” he added. “So my research is twofold: How do we pick it up earlier, and how do we reverse it? How can I put myself—as a clinician—out of business?”
Not Going Out of Business Yet
Even with the promise of newer, better treatments emerging from basic research, for now, the team will not be going out of business. Quite the opposite—with the growing reputation of the Heart Institute’s program and its growing patient volume, the group is physically expanding in the next five years, from the current two dedicated EP labs and a procedure room to a total of four labs.
“This field is going to grow,” said Dr. Nair. “More patients will be handled here as the burden of arrhythmias grows and more people are aware that something can be done. We’re doing complex and new ablation procedures that a lot of other centres don’t do.”
“Ablation will always be there,” added Dr. Redpath. “What we’re hoping for is that with the research we’re doing on the basic side, we’ll actually diagnose these people earlier, and we’ll offer treatments that delay or prevent the arrhythmias, and hopefully, reduce the need for ablation.
“And on the other hand, if we have to intervene, we’ll make better use of smarter devices, and we’ll be able to improve the quality and type of ablation that we give to people. So I see a very exciting future, where we’ll make real inroads into arrhythmia treatment.”