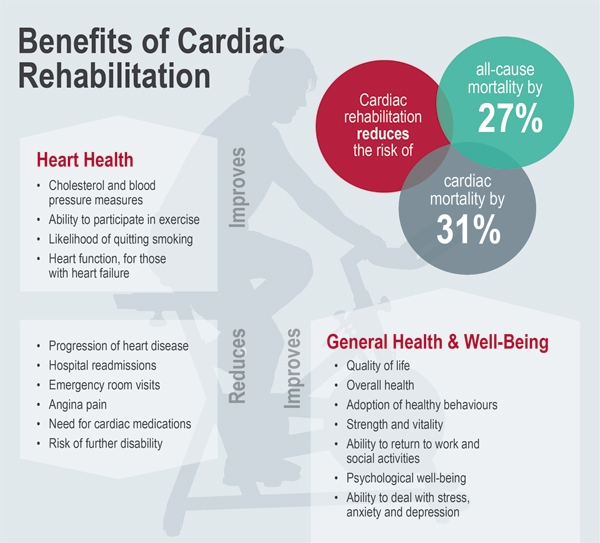
It’s been shown to lower death rates from heart disease and even from other causes after the onset of cardiovascular disease, and it helps patients achieve a better quality of life. In fact, cardiac rehabilitation is a key “next step” in the recovery process following a heart attack or procedures such as bypass surgery or angioplasty.
Indeed, with the benefits so attractive, you’d expect that patients would be lining up to take advantage of cardiac rehabilitation. But throughout North America, referral and participation rates are not optimal.
“Cardiac care is incomplete unless you’ve received the benefits of the secondary prevention programs delivered through cardiac rehabilitation,” said Dr. Andrew Pipe, Chief of the Division of Prevention and Rehabilitation at the University of Ottawa Heart Institute. “When you leave a dentist’s office, you have a card with your next appointment on it. We need to be doing the same.”
In an effort to improve those referral and participation rates—to make sure patients have that “next appointment”—Dr. Pipe’s rehabilitation group has implemented new approaches that are showing success.
The first step was to streamline the referral process. In 2006, the Heart Institute made referrals automatic. All inpatients would be referred for cardiac rehabilitation; the rehabilitation team would then determine eligibility.
The move to automatic referrals was effective at boosting the proportion of patients referred for rehabilitation, but it didn’t necessarily improve the proportion of patients actually enrolling in the program. So in 2008, the group made a second change by adding a new member to the cardiac rehabilitation team—a nurse, whose sole job would be to visit each patient at the Heart Institute and talk to him or her about rehabilitation.
Having this conversation is important, said acting Manager of Cardiac Rehabilitation Sueann Tiller. It helps patients understand the benefits of cardiac rehabilitation, and it aids them in overcoming barriers to participation.
It’s particularly important to talk to patients early in the process, explained Pamela Reid, one of the cardiac rehabilitation bedside referral nurses. In her experience, patients commonly go through a “honeymoon” stage, when they’re conscious that their lives were in danger and have been saved. At this point, they are committed to taking the steps necessary to improve their lives. Later on, she continued, after they’ve left the hospital, they get back into the pressures of their regular lives and the importance of rehab can fade.
It’s important to meet with patients early, before they’re back to their usual routines because there are very few people who don’t benefit from cardiac rehabilitation. Some patients may be too frail or physically disabled, or they may have so many co-morbidities that participation is impractical. Often, however, it’s the barriers patients erect themselves that make participation seem impossible.
Some patients, for instance, feel that what has happened to them is out of their control and there is nothing they can do to improve their situations. This absence of hope means that they don’t see any point in rehabilitation.
Other patients don’t see heart disease as the chronic condition that it is. They believe that their surgery or new stent has solved the problem and that there’s nothing more that needs to be done. In their minds, they’re cured.
“Cardiac care is incomplete unless you’ve received the benefits of the secondary prevention programs delivered through cardiac rehabilitation.” – Dr. Andrew Pipe, Chief, Division of Prevention and Rehabilitation, UOHI
Being able to talk directly with patients helps them overcome those barriers and find solutions that allow them to participate, Reid said. “When they’re giving me their host of reasons not to go to rehab, I try to have more reasons why they should go. I don’t think we’ve found a barrier yet that we haven’t figured out how to overcome.”
The effort to increase participation has paid off. According to an evaluation published this year in the Journal of Cardiopulmonary Rehabilitation and Prevention, having a bedside referral nurse more than doubled the proportion of eligible patients attending intake for the rehabilitation program, an increase from 15.5% of patients in 2003 to 2004 to 32.6% in 2008 to 2009.
With invention born of necessity, the Heart Institute has developed innovative ways to serve a younger and more geographically diverse population.
And when patients do participate, they quickly discover the benefits. The foundation of the program is a twice-weekly exercise class, led by physiotherapists who are all certified by the American College of Sports Medicine. Their work, though, is supplemented by a team of professionals, all with the same goal—to support patients in leading heart-healthy lives.
A dietitian offers nutrition workshops and one-on-one counselling to help patients eat healthily, including tips on grocery shopping, recipes and advice for eating out. A social worker or psychologist can help participants with the emotional and mental adjustments needed to live a full life while coping with a chronic disease. There’s even a vocational counsellor, something unique within cardiac rehabilitation programs in Canada, to help patients with the process of returning to work. This aspect is becoming increasingly important as the Heart Institute sees more and more younger patients.
And because the Heart Institute serves a large geographical area, it has had to be innovative in how it offers rehabilitation programs, Tiller said. In addition to the eight- to 12-week programs offered on-site, the Heart Institute provides a 12-week case-managed home program, where patients receive a binder of information that they work through with weekly phone calls from a member of the cardiac rehabilitation team. That program is also available in French, to better serve francophone patients within the region. A Tele-Rehab program connects classes in other centres through a video link to a class in session at the Heart Institute. That program, currently available in Cornwall, is in the process of expanding to Barry’s Bay.
A key focus of the on-site program is helping patients plan for the future. Staff work to link patients with Heart Wise Exercise programs located in municipal and private facilities in the community. These programs are offered by leaders who have been trained by the Heart Institute, ensuring a safe environment where patients can continue to get their heart-healthy physical activity.
“We’re hearing from patients what the gaps in service are,” said Tiller. “And we’re developing programs to close them.” This means there will be even fewer barriers to prevent patients from taking that important next step toward managing their own health.

