Martin Green, MD, vividly recalls the day in 1971 when he attended a medical school lecture on electrical activation of the heart, a subject that doctors and researchers were just beginning to explore.
“There were 225 people in the class and 224 of them walked out saying ‘That was the worst lecture I’ve ever heard,’” he recalled. “And one of them says ‘That stuff’s pretty cool.’”
Over the next 40 years, Dr. Green’s enthusiasm for the subject only increased. It became the foundation of a career rooted in helping the heart maintain a steady rhythm. Along the way, the field of cardiac electrophysiology (EP) grew from its infancy into a mature medical specialty.
A Developing Specialty
In the 1970s, EP consisted of little more than a basic understanding of the electrical pathways that were affected when the heart’s rhythm went awry. Few places in the world were focused on understanding and treating arrhythmias, which is why Dr. Green wound up in Maastricht in the Netherlands—arguably the birthplace of EP as a specialty.

There were also few drugs or surgical procedures at the time that could effectively deal with arrhythmias. “From a therapeutic point of view, we had no arrows in our quiver,” he acknowledged. “A lot of what we were doing then, we don’t do now, and almost everything we do now, we never even dreamed of then.”
Upon returning to Canada in 1983, he established EP as a new priority at the Ottawa Heart Institute by founding the Arrhythmia Service. By the early 1990s, he had been joined by electrophysiologist Anthony Tang, MD, and surgeon Paul Hendry, MD. Together, they would collaborate on the new technologies that were changing the way irregular heart rhythms could be corrected.
The foremost of these innovations was ablation, a method of delivering high frequency electrical energy from the tip of a catheter to destroy tissue in the heart causing an arrhythmia. This was a game-changer for EP, a powerful tool for tackling a growing challenge. As emerging treatments increasingly enabled individuals to survive major heart attacks and other forms of heart disease, these patients often developed arrhythmias caused by scarred and damaged cardiac tissue. Ablation could address these arrhythmias, but doing so required a better understanding of the key locations in the heart responsible for a steady beat.
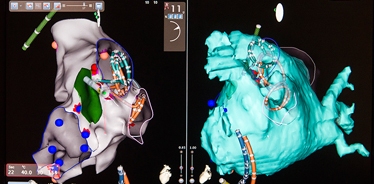
The advent of global positioning systems (GPS) in the 1990s offered a solution for mapping these locations. The same hardware that keeps us from getting lost on strange city streets also lets cardiologists map out the electrical dimensions of a patient’s heart. This capability has not only helped individual patients, it has contributed to EP’s larger understanding of how and where the heart’s electrical signals travel.
EP also benefited from the ever-shrinking scale of electronic equipment. Defibrillators, which deliver electrical stimulations to stabilize the beating of a racing or out-of-control heart, went from bulky surgical aids to compact implantable devices. By 2000, getting a pacemaker or defibrillator had become an outpatient procedure.
The use of implantable defibrillators to control the heartbeat came to be known as Cardiac Resynchronization Therapy. The success of CRT was confirmed in 2010 by the Resynchronization/Defibrillation for Ambulatory Heart Failure Trial (RAFT), a major long-term research study led by Dr. Tang and George Wells, PhD, at the Heart Institute. The findings indicated that, in comparison with other therapies, these implants reduced their risk of death by 24 per cent and changed the standard of care.
Sharing Knowledge and Expanding Expertise
With eight full-time electrophysiologists on staff, the Heart Institute now carries out more than 1,000 implantable device procedures every year, and more than 500 ablation procedures.
While the impact of new technology has undoubtedly been crucial to this expanding patient volume, Dr. Green has always regarded the need for expertise as paramount. For this reason, he initiated an EP fellowship program at the Heart Institute that attracts newcomers to the field from all over the world.
“I’ve had the opportunity to work for over 30 years now with some unbelievably good people,” he explained. “But I’ve also had the unbelievable opportunity to be involved in the training so many more good people.”
Although the Heart Institute has never advertised the program, it regularly draws dozens of applicants each year. Dr. Green has worked with upward of 40 fellows from locations as diverse as South Africa, India, Australia, Saudi Arabia, Kuwait, and Nepal, some of whom have returned to spearhead the growth of EP in their respective countries.
“If you ask me about my greatest accomplishment, it’s not me. It’s all these fellows, these people who are going out there and doing great things all over the world,” he insisted.
Closer to home, David Birnie, MD, director of the Arrhythmia Service, argues that Dr. Green’s dedication to the fellowship program reflects a passion that has improved EP at the Heart Institute in concrete ways. Throughout, he has championed collaboration and training.
“He really is respected all over the world for his leadership in this field,” said Dr. Birnie. “His skill in teaching is really remarkable.”
By way of example, he pointed to a relatively common form of arrhythmia called AV nodal tachycardia. Dr. Green learned how to treat this condition and then taught the procedure to everyone else on staff. The Heart Institute recently assessed 800 of its patient cases. The findings revealed the ultimate benefit of his teaching.
“The serious complication rate for this procedure worldwide is about 1 to 2 per cent,” said Dr. Birnie. “In our 800 patients, we had zero complications. That’s a major credit to Dr. Green’s skill. He learned it and passed it on to the rest of us.”
As he turns 65, Dr. Green has stopped performing clinical procedures. But he continues to see patients and he definitely plans to be available for consultation or advice. For all the progress he has seen since a boring medical school lecture changed everything for him, he expects much more to come.
“We’re good at some things, but we could be a whole lot better at others,” he concluded. “And there are things we’re only just getting good at and we’re not even close to great.”

