In the film Minority Report, the police were able to see who was going to commit a murder before it happened, and then prevent it. Being able to do the same thing for heart attacks would be a major advance for cardiology—knowing who is going to have a heart attack and then preventing it from happening.
A heart attack happens when plaque that has built up in the wall of a coronary artery develops a hard surface which cracks and ruptures. A blood clot forms at the site of the rupture and eventually blocks blood flow, depriving the heart of oxygen.
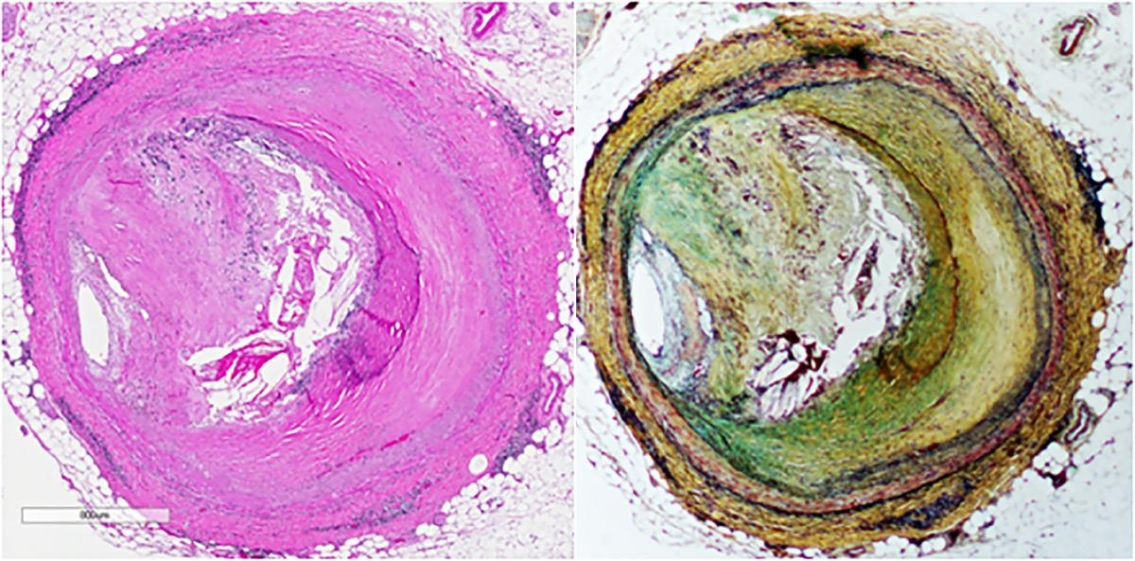
It’s not uncommon for people to have plaque in their arteries. The problem is that plaques don’t all behave the same way. Some simply sit there harmlessly, never causing a problem. These are called stable plaques. Others become unstable and result in a heart attack. The trick is how do you detect the vulnerable plaque that will rupture?
“It’s been an enigma... what it is about some plaques that do this and some that don’t,” said Katey Rayner, PhD, a researcher at the Ottawa Heart Institute.
Dr. Rayner’s group has found an answer to this conundrum that could be used to not only identify individual patients at high risk, but to find the specific location in their arteries where the heart attack would occur. They did this by coming up with a way to differentiate vulnerable plaques and then showing that non-invasive imaging can be used to identify them. The findings were published recently in the journal Science Advances.
One clue that led them in the right direction is that the so-called vulnerable plaques contain clusters of dead cells. But not much was known about the actual mechanisms triggering cell death, and there was no way to determine which plaques in a patient had the dead cell clusters.
“It’s kind of a Holy Grail in coronary artery disease to measure or detect plaques before they rupture, and before they become ones that actually cause heart attacks,” she said.
Another piece of the puzzle appeared about six years ago when Belgium researchers discovered that some cells in the body undergo a process of cell death called necroptosis—a process that was different from how cells usually die off in the body in that it caused inflammation.
Building on that, the Heart Institute researchers studied clusters of dead and dying cells in human plaque and discovered, for the first time, that they undergo this unusual necroptosis process.
They detected active necroptosis only in vulnerable lesions,and found that necrotic cores are active in humans with advanced atherosclerosis, she said. The findings opened the door to new ways of both diagnosing and treating vascular disease.
Necroptosis causes an inflammatory reaction. The plaque cells sit in an environment that is hostile to them and they respond to this by causing further inflammation which triggers a programmed cell suicide. Once enough cells die, the plaque becomes unstable. In other words, necroptosis underlies the plaques becoming vulnerable.
“Our work is the first to demonstrate that the necroptotic pathway is increased in vascular disease in humans,” said Dr. Rayner.
The question then was how could this information be used to help patients?
“We thought we would see whether we could visualize that process of necroptosis. If we could, the technique could be used to see which patients need to be treated more urgently,” she said. The work is still at a research stage, but provides a compelling target that could lead to a way of identifying which patients are at greater risk of heart attack and stroke—and help prevent those events from happening.
The next stage of the research was to use molecular imaging techniques to better understand what was happening within the plaque cells undergoing necroptosis. With molecular imaging, a chemical tracer designed to target and bind to specific types of cells is used. The tracer shows up as bright lights in the resulting images and helps researchers measure and observe what is actually happening in tissue samples.
This part of the work was made possible because the Heart Institute has a strong molecular imaging department. “We never would’ve thought to do it if it weren’t for the proximity of our neighbours who are molecular imaging people,” Dr. Rayner said.
A radioactive tracer attached to a compound, NEC-1, that binds specifically to necrototic cells was used. The resulting images using mouse tissue clearly showed unstable plaque.
Intriguingly, NEC-1 not only shows where necrotosis is happening in plaque, but it stops the activity and can stabilize the cell. This means there is a possibility for the development of a ‘theragnostic’—a compound that acts both as a tool that helps with diagnosis as well as a therapeutic. However, that is a long way off since the doses needed to do diagnosis and treatments are vastly different and there are various safety issues.
The next step is to improve the tracer and ensure its safety for use in humans. Eventually, the work may lead to a way to identify vulnerable plaque so patients can then be put on appropriate treatments to prevent them from rupturing and prevent heart attack and stroke.

