Sometimes, the smallest tools make the biggest difference. At the Ottawa Heart Institute, a fresh take on the humble hospital whiteboard is transforming how patients and care teams communicate.
With input from staff, patients, families, and design experts, the newly redesigned boards in in-patient rooms are supporting communication, reducing confusion, and helping patients feel more involved in their care.
A communication breakdown (and a simple solution)
Dry-erase boards were already present in in-patient rooms, but their use was inconsistent and lacked structure. The team recognized an opportunity to do better and improve communication across care teams.
The project launched in late 2023, sparked by an idea from Jennifer Bradley, a clinical manager at the Ottawa Heart Institute, and her colleagues.
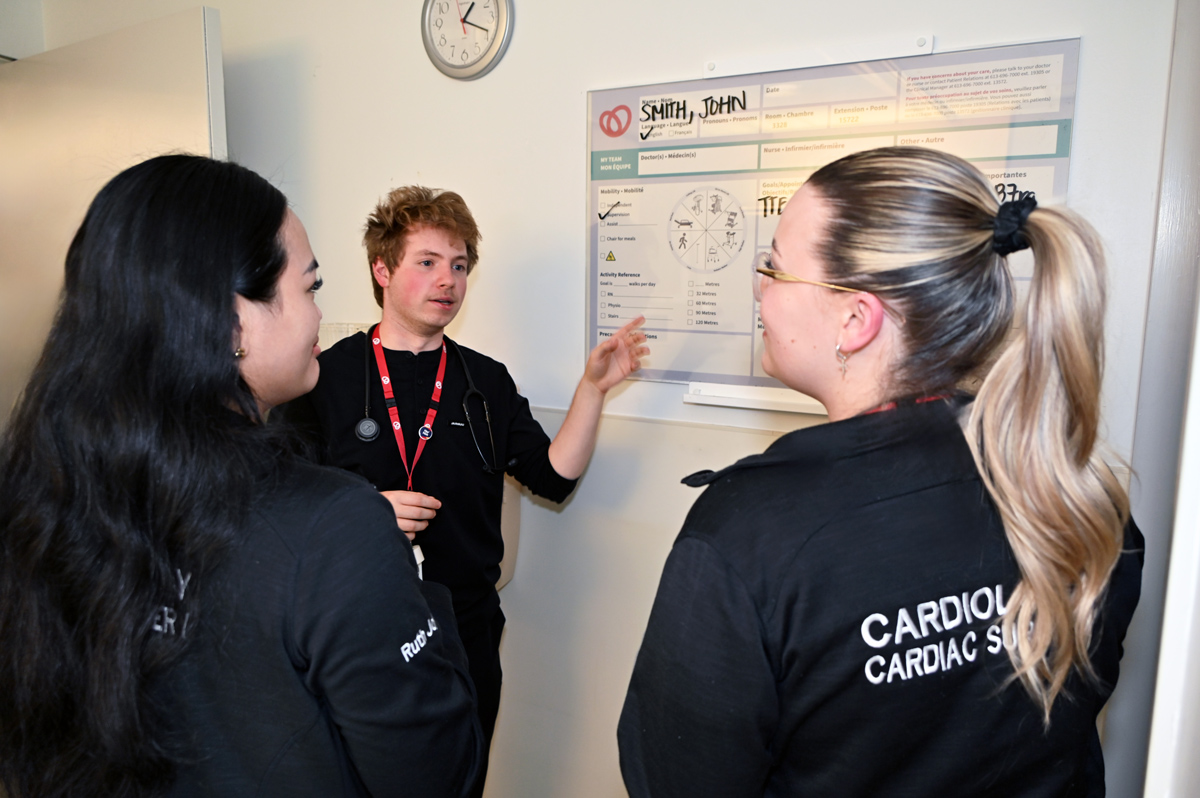
Nurses, allied health professionals, and physicians were often providing care for the same patients, though not always with the same information.
“We’re always looking for ways to strengthen how we connect with patients and with each other,” said Jennifer in an interview with The Beat. “It’s about making sure everyone has the right information at the right time.”
A staff and patient survey confirmed support for the idea to redesign the board. People wanted quick access to relevant information, written clearly, consistently, and in a way that made sense from the patient’s bedside.
Designed with patients, not just for them
The group established the Patient Whiteboard Committee. Membership included leaders, allied health professionals, nurses, a quality coordinator, and patient partners. Everyone brought a different lens to the project – and that was the point.
“Our aim was to create better communication between healthcare teams and patients by designing a clear, standardized patient whiteboard. We also wanted to encourage patients and their families to be actively involved in setting their care goals, while addressing any challenges in the system to make things run more smoothly,” said Jennifer Bradley.
For the patient partners, it was also about giving voice to the real concerns and needs of those receiving care.
“We suggested more space on the whiteboard to reflect patient and family member or caregiver questions and input. This is an opportunity to capture important questions as the day unfolds, so these are not forgotten when the doctor does their check-in with the patient,” one patient partner shared.
“We also felt it was important to include information to help the patient manage their care, such as upcoming tests and procedures, discharge plans and who to contact if you have concerns about your care. We suggested adding space for the name of the patient's doctor as well as the nurse on shift. When patients are feeling vulnerable in a hospital room where so much is outside your control, having this information on the board can be reassuring.”
Designed with heart
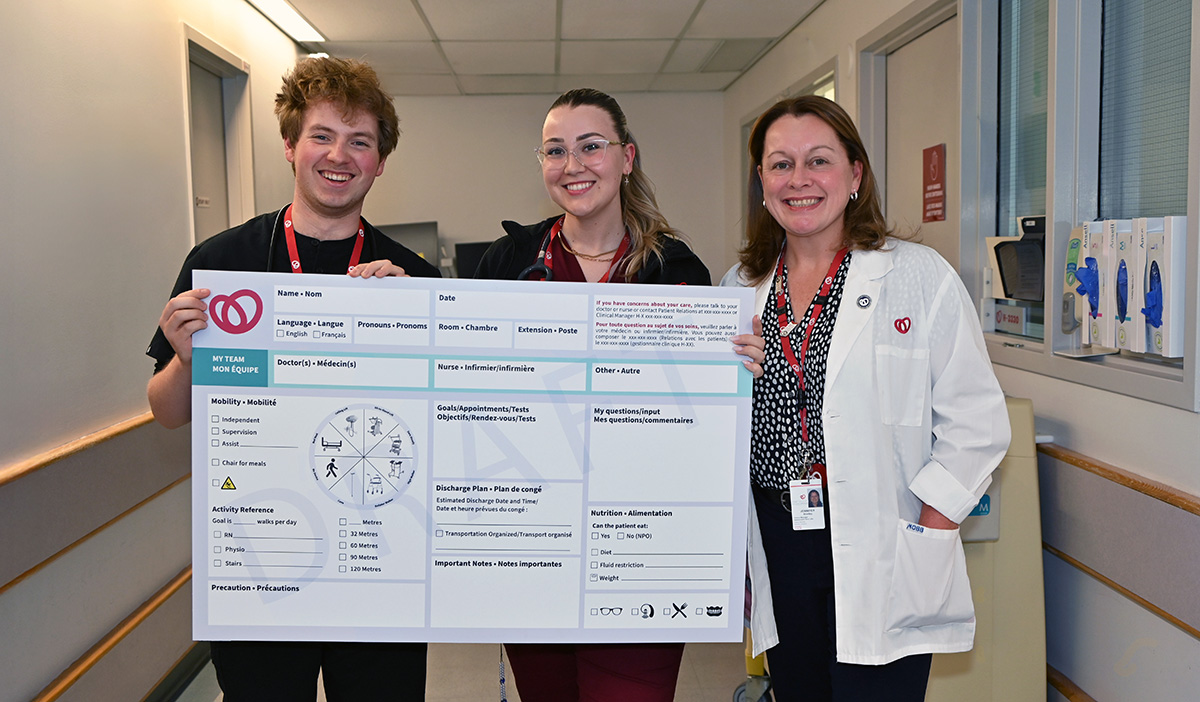
Angela Poitras, the Ottawa Heart Institute’s brand and design lead, translated the group’s ideas into multiple design drafts. Colour, font size, accessibility, and clarity were all reviewed closely. Even the viewing angle from a hospital bed was tested.
"We didn’t just want it to look nice—we wanted to make sure it worked in real life for patients with visual impairments, for multilingual families, and for staff who only have 30 seconds to glance at it and get key information," Angela explained.
The committee’s insights led to the inclusion of a daily schedule, visual icons for mobility aids, space for preferred names, languages and preferred prounouns, and clearly labelled sections for upcoming tests and dietary needs. Their lived experiences ensured the design reflected what patients truly need in moments of uncertainty.
“It was an opportunity to work collaboratively with a team of allied healthcare professionals who are all very dedicated and committed to making the patient experience better,” one patient partner said.
“Compromises had to be made given the long list of needs and the limited space on the board. But by being involved throughout the process, we were able to continue to highlight issues or concerns that are important to patients.”
Piloted, perfected, and put into action
Jennifer Bradley and her team launched a pilot of six boards on one of the wards and tested it for eight weeks in early 2025. Feedback was collected from patients, families, and staff, and the design was refined one final time.
Full installation began in March. Now, 96 new boards are in place across three care units across the Heart Institute. Staff are encouraged to update the boards at the start of every shift. The change has been felt almost immediately.
“We’re receiving positive feedback from our patients and families, and fewer surprises for staff,” Jennifer said.
It’s helped make care feel more personal and more transparent. Allied health professionals say the boards help close communication gaps when face-to-face conversations aren’t possible. And while tools like Epic – comprehensive software for managing electronic health records – remain essential, the boards offer a quick, real-time reference for what matters now.
Small changes leading to better care for everyone
The success of the project, Jennifer Bradley said, is thanks to strong collaboration across departments.
“This started small,” Jennifer reflected. “But it’s become something truly meaningful. It shows what’s possible when you listen, collaborate, and care about the details.”
Now, critical care teams are exploring how to adapt the model for their unique environments.
And it all started with a marker and a fresh perspective.
Never miss a Beat
Want interesting stories like this delivered straight to your inbox as they happen?
Subscribe to our mailing list