Coronary artery disease (CAD) is a condition which affects the arteries that supply the heart with blood. It is usually caused by atherosclerosis which is a buildup of plaque inside the artery walls. This buildup causes the inside of the arteries to become narrower and slows down the flow of blood.
There are many risk factors for CAD, Some are not controllable, but others can be modified. CAD develops over a long period of time and eventually progresses to the point where you may feel symptoms such as chest pain. Diagnosis is made using various tests such as an electrocardiogram (ECG) or a stress test. Treatment for CAD includes lifestyle changes, medications, and sometimes, cardiac procedures or surgery.
About Coronary Artery Disease
The heart is a muscle which pumps blood around the body through a network of blood vessels called arteries.
The left side of the heart receives fresh, oxygen-rich blood from the lungs and then pumps it out through a large artery called the aorta. The aorta branches into smaller arteries that go to all parts of the body. The various parts of the body take the oxygen out of the blood. The now stale, oxygen-poor blood is returned to the right side of the heart through blood vessel called veins. The right side of the heart pumps this stale blood to the lungs where it picks up more oxygen and the cycle begins again.
The Coronary Arteries
The heart muscle, like every other part of the body, needs its own oxygen-rich blood supply. Arteries branch off the aorta and spread over the outside surface of the heart feeding oxygen to the muscle. The right coronary artery (RCA) supplies the bottom part of the heart. The short left main (LM) artery branches into the left anterior descending (LAD) artery that supplies the front of the heart and the circumflex (Cx) artery which supplies the back of the heart.
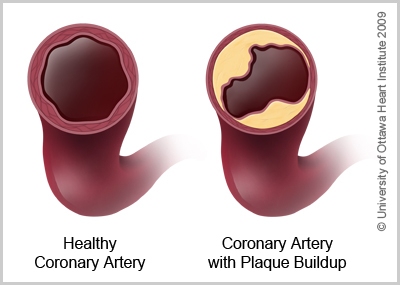
In coronary artery disease, there is a blockage in the arteries that supply blood and oxygen to the heart. The most common cause is atherosclerosis which is a buildup of plaque inside the walls of the arteries.
Plaque is made of several substances including cholesterol. Plaque buildup can start at an early age and is caused by a combination of genetic and lifestyle factors that are called risk factors. As plaque builds up over time, the arteries become increasingly narrow. Eventually, blood flow to parts of the heart is slowed or blocked.
Poor blood flow to the heart can cause angina. Blood clots are more likely to form in arteries which have reduced blood flow, which then further block the arteries. CAD can eventually lead to unstable angina or a heart attack.
On this page
Causes
Coronary artery disease is caused by a combination of genetic and lifestyle factors. These are called risk factors. The following risk factors are important to be aware of, but are not considered to be controllable:
- Age: As you get older, your risk of heart disease increases
- Gender:
- Men: Men over the age of 55 are at higher risk of heart disease
- Women: After menopause, a woman’s risk of heart disease gradually increases until it becomes the same as a man’s
- Heredity: Your risk of heart disease is increased if close family members—a parent, brother or sister developed heart disease before age 55 or, in the case of female relatives, before menopause.
- Ethnicity: First nations people and people of African or Asian descent are at higher risk of developing heart disease than other groups.
The risk factors that you can control are:
- Smoking
- Excess body weight, especially around your waist
- Diabetes
- High blood pressure (hypertension)
- Abnormal blood cholesterol levels
- Lack of regular exercise
- Excessive stress levels
- Depression
These are modifiable risk factors.
Diagnosis
Tests commonly used to diagnose CAD include:
- Electrocardiogram: to identify problems with heart rhythm or signs of a heart attack
- Treadmill testing: to measure how well the heart functions when challenged to work harder than normal (during exercise)
- Nuclear perfusion imaging: to identify areas of the heart that are receiving less blood
- Echocardiogram: to determine the volume of blood pumped by the heart. This test may be done during exercise or after the administration of medication to stimulate the heart
- CT coronary angiography: to identify blockages in the arteries in the heart
- Cardiac catheterization: to identify blocked or restricted arteries
Symptoms
CAD usually has no symptoms for several years during its early stages. Eventually, the disease progresses until the symptoms of angina or heart attack occur. These symptoms can be experienced during activity or at rest:
- Chest pain, or a feeling of heaviness in the chest
- Pain in the arm, neck or jaw
- Shortness of breath
- Sweating
- Nausea
- Heart palpitations (a racing or irregular heartbeat)
- Loss of consciousness
For women, the signs of heart attacks in women can be far more subtle. Early signs in women include:
- Fatigue: A significant change in energy level, something out of the norm that lasts more than a few days. At 70%, unusual fatigue is the single most common long-term symptom for women.
- Sleep difficulties: Trouble falling asleep, or waking up in the night more than usual, often because of an ache or pain that won’t let you sleep.
- Shortness of breath: Becoming winded doing the most basic activities, but especially during exercise.
- Indigestion: Feeling uncomfortably full soon after eating, sometimes with pain or burning in the upper abdomen.
- Chest discomfort: It may be mild discomfort, it may seem like indigestion.
- Anxiety: Feeling nervous or apprehensive for no apparent reason, or more than usual.
Symptoms women commonly experience when a heart attack occurs include:
- Chest pain: While men having a heart attack often report a crushing or stabbing pain in their chest, many women say they felt pressure, tightness or aching in their chest or back.
- Fatigue: More than feeling tired, this overwhelming fatigue makes it hard to do anything.
- Breathing difficulties: It’s suddenly a struggle to take a full breath.
- Radiating pain: Pain spreads across the jaw, arm, shoulder or radiating across the back
Anyone who thinks they are having a heart attack should call 911 or go immediately to an emergency room.
Treatments
Treatments for CAD usually include lifestyle changes and medications, sometimes in combination with cardiac procedures or surgery. The best treatment combination will be determined based on your individual circumstances.
Medications
There are many medications that can help coronary artery disease. Your doctor will likely prescribe a combination of medications which will work to:
- Lower the workload of your heart
- Help relax the blood vessels
- Lower cholesterol
- Help prevent blood clots from forming
- Lower the overall risk of you having a heart attack
You will be taking these medications for the rest of your life.
Cardiac Procedures: Sometimes an angiogram is needed to show the blockages and determine whether medications are sufficient for treatment or whether an angioplasty (the use of a balloon to open the blockage) and stent (a wire mesh tube to keep the artery open) are required. Sometimes coronary artery bypass surgery is necessary to attach new arteries or veins to go around the blockages.
Lifestyle Changes
To manage CAD, it is important to:
- Quit smoking because cigarette smoking narrows the blood vessels. Smoking-cessation aids are available to patients who find it difficult to quit on their own.
- Get your cholesterol checked and get high cholesterol under control.
- Eat a healthy diet low in saturated fat, cholesterol, and salt.
- Exercise regularly.
- Maintain a healthy weight. Losing weight if you are overweight, reduces the burden excess weight places on the heart. Regular exercise can help control weight and reduce other risk factors for CAD, such as high blood pressure.
Resources
- Coronary Artery Disease Patient Guide
- Coronary Artery Disease - Treatment options: A Heart Team Approach (PDF)
- UOHI video series: Coronary Artery Disease and Recovery from a Heart Attack - Care after Discharge
Risk Factors for Cardiovascular Disease
Learn about risk factors for heart disease and strategies for managing them to improve your overall heart health.