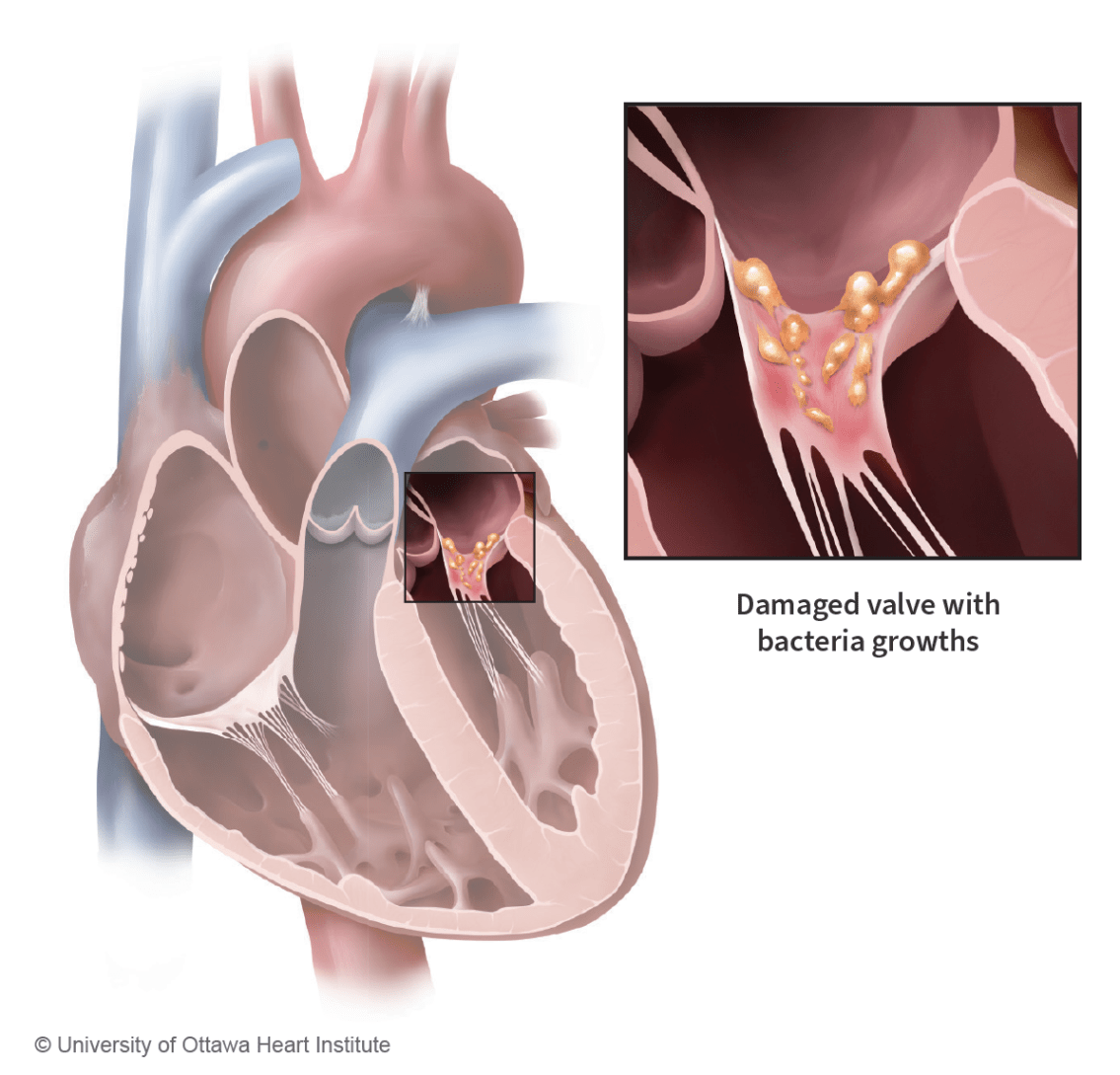
Infective endocarditis is an infection of the inner lining of the heart and its valves. The infection is caused by microorganisms (bacteria or fungi) that can enter the bloodstream from another part of your body, such as through the mucous membranes of the mouth or through an open wound.
Normally, microorganisms that enter the bloodstream pass harmlessly through the heart and are killed by the immune system. However, microorganisms circulating in the bloodstream may adhere to heart tissue. When this happens, they can hide from the immune system and cause a life-threatening infection.
On this page
What are the symptoms of infective endocarditis?
Diagnosing infective endocarditis is often difficult because symptoms may mimic the flu or viral infections, and even menopause symptoms like night sweats.
The most common symptoms of infective endocarditis are:
- Fever and/or persistent fever for no known reason
- Recurrence of fever after treatment of a recent infection
- Chills
- Sweating or night sweats
- Fatigue
- Muscle and joint aches and/or pain
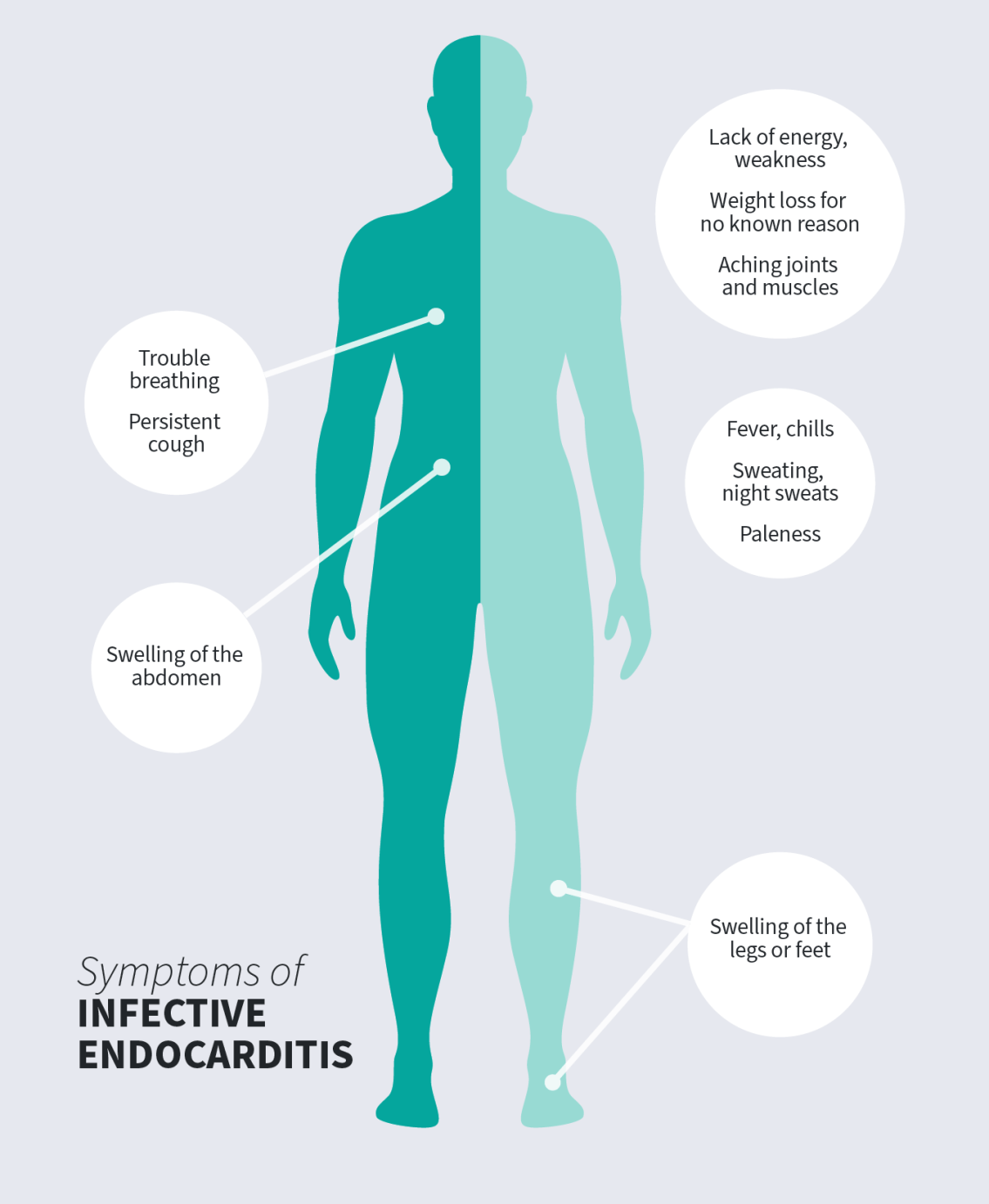
Other symptoms can include:
- Small areas of bleeding under the nails (splinter hemorrhages)
- Red, painless spots on the palms of the hands and soles of the feet (Janeway lesions)
- Red, painful lumps in the pads of the fingers and toes (Osler’s nodes)
- Tiny purple or red spots on the skin, whites of the eyes, or in the mouth
- Trouble breathing
- Persistent cough
- Weight loss for no known reason
- Swelling of the feet, legs, or abdomen
Symptoms of infective endocarditis can develop quickly (within days) or slowly (over weeks or months). If you think you have an infection, see a doctor or your healthcare team as soon as possible. This can prevent further problems.
What are the risk factors for infective endocarditis?
Infective endocarditis is an uncommon condition. Although it can occur in patients with normal hearts, people with heart abnormalities (known or unknown/diagnosed or undiagnosed) are at higher risk of developing infective endocarditis.
You can have a higher risk of developing infective endocarditis if:
- You have had infective endocarditis before.
- You have an artificial heart valve. This means you have had a procedure or a surgery to repair or replace one of your heart valves.
- You have an implanted heart device, such as a pacemaker.
- You have congenital heart disease (meaning you were born with a heart disorder) or you had surgery for congenital heart disease in the last six months.
- You use intravenous (IV) drugs. This includes reusing needles or other injection supplies, injecting into skin that has not been cleaned, and/or injecting substances that have not been totally dissolved.
- You had a heart transplant.
- You have long-term intravenous (IV) catheter use, such as with chemotherapy or hemodialysis.
- You have heart valve disease.
What are the complications of infective endocarditis?
Infective endocarditis can lead to other life-threatening conditions including:
- Stroke or reduced blood flow to other organs. This can occur when clumps of bacteria break off from the heart and block the blood vessels.
- Tissue damage, including a blood clot in the lungs (pulmonary embolism) or other organs.
- Permanent damage to the heart valves (with uncontrolled infective endocarditis), eventually leading to heart failure.
- Infective endocarditis is a severe disease and can be life-threatening.
How is infective endocarditis diagnosed?
If your doctor believes you may have infective endocarditis, they will order one or more of the following tests:
- Blood tests: Blood tests may show an elevated white blood cell count or microorganisms in the blood. They should be done before giving antibiotics, which can mask an infection.
- Transthoracic echocardiogram (TTE): Ultrasound examination of the heart that looks at the heart valves and heart function. It is usually done with a probe placed on the chest wall, often as an initial test.
- Transesophageal echocardiogram (TEE): Often needed so your healthcare team can see your heart more clearly than with a transthoracic echocardiogram. This test involves inserting a special probe through the mouth and into the esophagus (like an endoscopy).
- Electrocardiogram (ECG): Identifies problems with heart rhythm and injury caused by a possible infection.
- Fluorodeoxyglucose positron emission tomography (FDG-PET) scan: A test that uses a radioactive substance similar to sugar to detect areas of high metabolic activity in the body, including infections. This test is used to confirm the diagnosis of infective endocarditis when other tests are inconclusive.
- Computed tomography (CT): A special test that uses X-rays or imaging to show details of the heart, sometimes needed to confirm the diagnosis of infective endocarditis. This test looks for physical damage to the heart and/or other organs.
Your healthcare team will talk to you about which tests are right for you. If you have any questions about any of the tests, please speak with your healthcare team.
What is the treatment for infective endocarditis?
There are two options to treat infective endocarditis:
Drug therapies:
- High doses of antibiotics or antifungal medication(s) delivered into a vein by intravenous (IV) line.
- Treatment usually lasts four to six weeks.
- Drugs are started in hospital. Some patients finish the treatment at home, under the supervision of a home care team, or at a community clinic or their family doctor’s office.
Surgery:
- Surgery can be used to remove tissue infected by highly damaging bacteria or fungi.
- Sometimes, the heart valve needs repair or replacement.
How can you reduce your risk of infective endocarditis?
You can reduce your risk of infective endocarditis by taking these steps:
- If you have one of the conditions that puts you at a higher risk of infective endocarditis, you must tell your dentist. Your dentist or family doctor should prescribe a preventive antibiotic before any dental procedure, including a cleaning.
- Practice good oral hygiene daily by brushing and flossing to improve your dental and heart health. Visit your dentist regularly as recommended.
- If you are booked for any medical procedures that could cause bacteria to enter the blood stream, such as biopsies, discuss your risk of infective endocarditis with your healthcare team.
- Avoid cosmetic procedures, such as piercings or tattoos, which can push bacteria from the skin into the bloodstream.
- Pay careful attention to any sign of infection like a fever, abscess, or urinary tract infection. If you suspect infection, see your healthcare team as soon as possible to prevent further problems.
- Avoid using intravenous (IV) drugs. For information on safer substance use, visit CATIE or contact your local public health unit. To learn more about treatment options for substance use disorder, visit AccessMHA or contact your primary care provider.
Know the signs and symptoms of infective endocarditis such as fever, chills, or unexplained weight loss, and see your healthcare team as soon as possible if you suspect you may have infective endocarditis. Ask your healthcare provider if blood cultures should be taken before taking antibiotics.