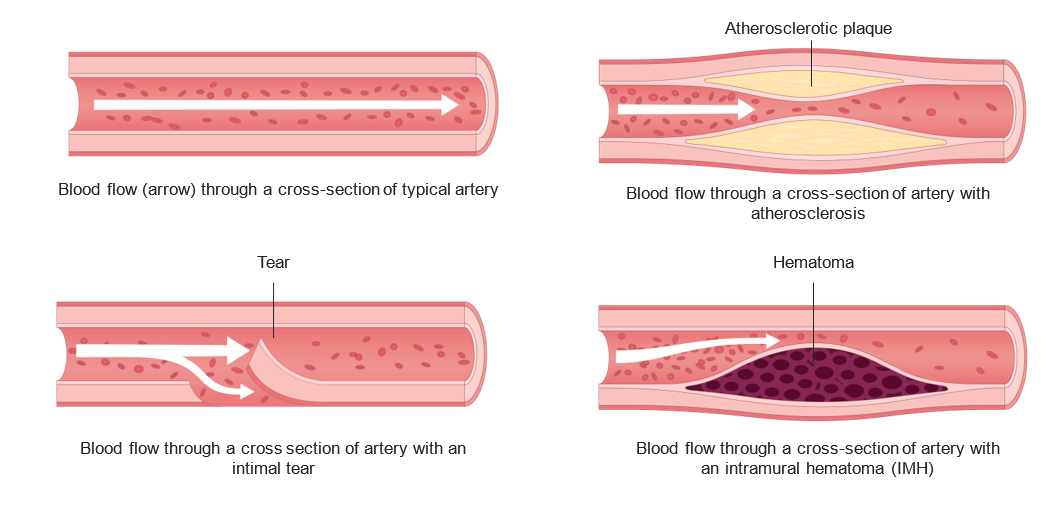
Spontaneous coronary artery dissection (SCAD) is a type of heart attack that occurs when there is a sudden tear (a dissection) in the wall of a blood vessel (an artery) in the heart.
This tear can happen in the inner layer of the artery or between its layers. When this happens, blood can build up inside the wall of the artery (called a hematoma), which may partly or fully block blood flow. This blockage can lead to a heart attack (or “acute myocardial infarction”).
What is the difference between SCAD and a “classic” heart attack?
SCAD is different from a traditional—or “atherosclerotic”—heart attack, although both have similar consequences. An atherosclerotic heart attack is caused by a buildup of cholesterol plaque in the arteries of the heart. When a plaque suddenly breaks off or ruptures, a clot forms inside the artery, which blocks blood flow. Atherosclerotic heart attacks do not involve tearing of the artery.
Even though SCAD and atherosclerotic heart attacks have different causes, they can lead to the same serious problems, including:
- Permanent damage to the heart muscle
- Irregular heartbeats (arrhythmias), which can be life-threatening
- Cardiac arrest (when the heart suddenly stops beating)
Who can have SCAD?
Both women and men can experience a SCAD heart attack. SCAD occurs more often in women, who account for about 90% of cases.
The average age of people diagnosed with SCAD is between 44 and 53, but it can occur at any age. SCAD used to be considered rare, but we now know that it accounts for about 4% of all heart attacks worldwide.
Among women 50 years of age and under, SCAD is the cause of 35% of heart attacks. SCAD is also the number one cause of heart attacks in pregnancy. SCAD can recur in 8% to 27% of cases. Research is still ongoing to better understand recurrence rates.
On this page
Signs and symptoms
Like other types of heart attacks, SCAD can cause chest pain, pressure and/or tightness. Other symptoms include:
- Rapid heartbeat/ racing heart
- Pain in arms, shoulders, jaw, neck or stomach
- Shortness of breath
- Sweating
- Headache
- Nausea and vomiting
- Dizziness or light-headedness
- Back pain
- Unusual, extreme tiredness
- Fainting
Although unusual, SCAD may cause more serious symptoms, including:
- Abnormally fast and life-threatening heart rhythm
- Cardiogenic shock (when the heart cannot pump enough blood to the rest of the body)
- Cardiac arrest or sudden death
Although not well understood at this time, up to 70% of patients experience recurrent chest pain in the initial months after a SCAD. Some female patients experience episodes of chest pain associated with their menstrual periods (“catamenial angina”).
It is important to discuss with your healthcare team what to do if you have chest pain following a SCAD. Medication such as nitroglycerin may be prescribed to relieve chest pain. For many patients with recurring chest pain after a SCAD, the pain resolves after a few weeks or months following the initial event.
Causes and risk factors
Although research is ongoing, it is still unclear what causes SCAD. Several risk factors have been identified.
- Being female: SCAD can occur in both women and men, but women are at higher risk.
- Fibromuscular dysplasia (FMD): FMD is a rare condition that causes irregular growth of cells in the walls of one or more arteries. This can weaken the artery walls and reduce blood flow. FMD can also cause high blood pressure, stroke and tears (dissection) in other blood vessels in the head, neck, kidneys, abdomen, and legs. FMD has been found in more than 70% of patients with SCAD.
- Hormonal changes: There may be a connection between SCAD and female hormones given the higher prevalence in females in general, and the high rates in pregnant women, women who have recently given birth, and perimenopausal women. There is still more research being done to explore the connections with hormonal contraception and hormone replacement therapy.
- Extreme emotional stress: Many people have reported severe emotional anxiety or stress (e.g., from receiving bad news, employment-related stressors, losing a loved one, a major medical diagnosis, loss of a job or a relationship) in the period before their SCAD. This is especially common in women.
- Extreme physical stress: Extreme physical effort, such as intense aerobic or weight-training activity, has been reported in the period before SCAD. This is more common in men.
- Connective tissue disorders: SCAD has been reported in several disorders that affect the connective tissues in the body, such as Marfan syndrome, Ehlers-Danlos syndrome, and Loey-Dietz syndrome. More research is needed to understand this.
- Genetics: The genetics of SCAD is not well understood. Only around 3.5% of cases are due to rare genetic abnormalities. A few genes are associated with SCAD. The familial genes F11R and TLN1, a variant PHACTR1 gene, COL3A1, and COL5A1 genes have been implicated. Novel tissue factor gene F3, which is part of a blood-clotting pathway, has also been associated with higher risk for SCAD. Further research is needed to identify more associated genes and understand whether there is a clear genetic component to SCAD.
Diagnosis and treatment
Diagnostic tests
The first tests used to help diagnose SCAD are an electrocardiogram (ECG) and blood work, specifically troponin levels. A coronary angiogram will be done next, and a CT scan may also be used. These are the main tests used to diagnose SCAD.
During an angiogram, the doctor will insert a long, thin tube (catheter) into an artery in the groin or wrist. The catheter is then guided to the damaged coronary artery using X-rays or other imaging tests.
Treatments
Your treatment depends on your specific situation. Consideration is given to the size and location of the tear in the artery, possible damage to the artery or heart muscle,
and your symptoms. Whenever possible, doctors allow the damaged artery to heal
on its own.
Unlike other types of heart attacks, there are risks to stenting arteries in SCAD patients, including the risk of extending or worsening the dissection. However, when
necessary, doctors will resort to a stent or cardiac surgery.
Percutaneous coronary intervention (PCI)
During your angiogram, the doctors will be able to see where the SCAD occurred. When needed, doctors may perform a PCI, also known as an “angioplasty” or “stenting”. During this procedure, the doctor passes a small balloon through the catheter to open the blocked portion of the artery. They may place one or more tiny mesh tubes (called a stent) inside the artery to hold it open and restore blood flow to your heart. The doctor inflates the balloon, expanding the stent against your artery walls. The stent is left in place to hold the artery open. If you were treated with one or more stents, more information will be provided to you.
Cardiac surgery
If other treatments have not worked, and the SCAD is immediately life-threatening, surgery may be the best treatment. On rare occasions, coronary artery bypass grafting (CABG) may be used to create a new passage for blood to reach your heart.
CABG is a procedure that involves removing a blood vessel from another part of your body, such as your chest wall or leg. That blood vessel is stitched onto the coronary artery to bypass blood flow around your damaged artery. If this treatment is recommended for you, more information will be provided to you by a surgeon.
Medication therapy
After a SCAD, your doctor may prescribe medications to restore blood flow and
promote healing. These medications may be temporary or permanent, depending
on your personal situation. Research is still ongoing to determine the best medications after a SCAD event.
Here are some medications you may be prescribed:
- Anti-platelet agents to reduce the number of blood-clotting platelets in your blood and lessen the risk of a clot forming in your torn artery. The most used anti-platelet agent is aspirin. You may also be prescribed an additional anti-platelet agent, such
as clopidogrel or ticagrelor, for up to one year after your SCAD. - Beta-blockers to make your heart beat more slowly and with less force. This decreases the pressure on the torn vessel and promotes healing. Research has shown that SCAD patients who were taking beta-blockers had a lower risk of SCAD recurrence than patients who were not taking these medications.
- ACE inhibitors to open the blood vessels leading out of the heart, which decreases the workload of the heart muscle. This type of medication is prescribed if your blood pressure is too high despite your other medications, or if the SCAD caused heart damage, thereby weakening the heart muscle.
- Nitroglycerin spray to open blood vessels. This is prescribed in case you have a recurrence of chest pain. If you have been prescribed nitroglycerin spray, the NitroAssist application can help you use it correctly.
Medications may relieve symptoms and promote healing. If chest pain or other symptoms continue, your doctor will discuss treatment options with you.
Some medications should be avoided after a SCAD. Speak to your doctor before taking triptans for migraines, stimulants (including cocaine), and hormonal therapy.
The way forward: building your recovery plan
The University of Ottawa Heart Institute offers several resources. Many services do not require a referral. For those that do, please speak to your doctor.
“Living with SCAD” class
We offer a monthly “Living with SCAD” class to support SCAD survivors between the time they leave the hospital and their first follow-up appointment. It is a virtual group presentation followed by a question-and-answer period with an advanced practice nurse and a physiotherapist.
Cardiac rehabilitation
This exercise and education program is designed to help you recover in a safe environment. You can resume your regular activities with medical oversight, regardless of your fitness level. Our nurses and physiotherapists are experienced in rehabilitation guidelines and recommendations after a SCAD.
Mental health and psychology services
Some patients experience anxiety, depression, post-traumatic stress disorder (PTSD) or stress after a SCAD. As part of our cardiac rehabilitation program, psychology services are available to help you with cardiac-related concerns. Ask for a referral from your healthcare team.
Diet and nutrition
During your appointment with Cardiac Rehabilitation or the Women’s Heart Health Clinic, healthcare providers will review your cholesterol numbers and your diet to assess whether seeing a dietician would benefit you. Eat healthy to maintain your cardiovascular health and watch our educational videos to help you get started. Also follow our Top 10 Tips for Healthy Eating
Quit smoking
Avoid smoking cigarettes or e-cigarettes. If you have not been referred to the Quit Smoking Program, we have specialists at the UOHI who can help you cut down or quit smoking. Call 613-696-7069 to self-refer.
Talk to your kids
Many patients with SCAD are young and have children. Many are unsure of how to discuss their heart condition with their kids. Please see our guide Discussing your Heart Condition with Children and Youth.
Women@Heart peer support program
The Women@Heart SCAD program is a virtual, structured, group-based peer-support program for women with SCAD, led by trained fellow SCAD survivors. SCAD patients find it extremely helpful to connect with others who have experienced something similar. Visit the program’s webpage to learn more and sign up.
Women’s Heart Health Clinic (WHHC)
Patients with SCAD may be referred to this clinic for ongoing care after their hospital stay. Specially trained nurses and doctors monitor your SCAD on an ongoing basis. The Women’s Heart Health Clinic also offers educational classes to our patients to help them stay informed about SCAD and healthy living.
Staying active safely after SCAD
After SCAD, the goal is to stay active for heart and mental health, without overstressing the arteries. Tips for resuming regular activities:
- Attend cardiovascular rehabilitation for specific guidance.
- Resume physical exercise slowly.
- Do not lift more than 20 to 30 pounds until your doctor clears you to do so.
- Avoid isometric (heavy weight or resistance-based) exercise and straining to lift heavy objects until you speak to your specialist.
- If you have FMD or dissections in the head or neck, avoid:
- Push-ups, sit-ups, or other exercises that involve straining your muscles against heavy resistance.
- Extreme head or neck positions, contortions, or manipulations.
Recommended:
- Cardiovascular rehabilitation
- Moderate aerobic exercise
- Interval training
- Strength training with light weights and high repetitions
With caution:
- Aerobic exercise to build endurance
- Strength training for muscle building
- Yoga (without extreme head and neck positions)
Avoid:
- Sudden or very intense exercise
- Lifting very heavy weights while holding your breath
- Contact sports
- Extreme head or neck positions
Source: Tweet, M.S., et al. (2021). Physical activity and exercise in patients with spontaneous coronary artery dissection and fibromuscular dysplasia. European Heart Journal, 42(37), 3825–3828.
Living with SCAD
When you leave the hospital, your dissection will still be healing. You should take precautions to ensure your heart is protected while it heals.
Medications
Understand your medications and why they have been prescribed. Take your medications as directed and discuss any side effects or other concerns with your doctor. Do NOT stop taking them without consulting with your doctor.
Activities of daily living
Most people can resume cooking, doing laundry and grocery shopping gradually over the first week or two. You may need to limit yourself to lighter grocery bags or laundry hampers. Take breaks as needed and listen to your body.
Driving
Ask your cardiologist when you can drive again. The time you need to wait before driving after a heart attack depends on your ejection fraction (EF), the measurement of the percentage of blood leaving your heart each time it beats. Your cardiologist will use your EF to determine when you can safely drive again. It can vary from two weeks to three months from the time of your heart attack.
Below are some general guidelines. Please talk to your cardiologist to find out when you can drive safely after your heart attack.
If your ejection fraction is 41% or more:
- You must wait two weeks before driving again.
- If you drive for a living, you must wait one month before driving again, unless your cardiologist instructs otherwise.
If your ejection fraction is 40% or less:
- You must wait one month before driving again.
- If you drive for a living, you must wait three months before driving again, unless your cardiologist instructs otherwise.
Sexual activity
If you can walk up a flight of stairs, you can usually engage in sexual activity. For most patients, this starts around four to six weeks after a heart attack. Please speak to your doctor about when it would be safe for you.
Pregnancy
It is recommended that patients who have had a SCAD avoid becoming pregnant due to the high risk of recurrent SCAD heart attacks. Pregnancy-associated SCAD is often more aggressive and more severe than SCAD not associated with pregnancy. Use appropriate and reliable birth control methods (as recommended by your doctor) to prevent pregnancy until you have discussed the risks of future pregnancy with your doctor. Avoid contraceptives with estrogen. Recommended methods of birth control include progesterone-based or copper-based intrauterine devices (IUDs), progesterone-containing subdermal implants, tubal ligation, or vasectomy. Barrier methods such
as condoms or diaphragms are not considered adequate.
Self-care
Take care of yourself and listen to your body. Rest when you need to, sleep well, eat well, exercise as instructed, spend time with family and friends, and find healthy ways
to cope with stress. Check out our top 10 tips for activity, sleep, stress, emotional health and healthy eating.
Preparing for your appointments
Care protocols for patients with SCAD are updated as research advances, so doctors welcome any questions about new information. You may find the information changes over time because of this ongoing research.
Feel free to bring someone with you to your appointments if you want support.
To get the most from your appointments, it helps to make a list of questions or concerns ahead of time. Below are some common questions asked by SCAD patients like you:
- What caused my SCAD?
- Do I need any more tests?
- What alternative treatments are available in my situation?
- What is my risk of having another SCAD?
- How will my SCAD impact my other health conditions?
- Are there restrictions I should follow (such as lifting, heart rate limits, isometric or inversion exercises)?
- Is it safe for me to become pregnant?
- Should I be tested for any other conditions?
- Why am I taking the medications I have been prescribed?
- If I experience side effects from my medication, what should I do?
- How do I know if my symptoms are an emergency?
- When should I have a follow-up appointment, and who will schedule it?
Videos: Frequently asked questions about SCAD
Watch these videos directly on YouTube.
What is a SCAD and how is it different from other forms of heart disease?
I was fairly healthy before my SCAD event and I didn’t have any warning signs, what might have caused it?
People talk about a link between SCAD and FMD – What is that and should I worry about it?
I heard that people with blocked arteries receive stents at the time of a heart attack, but I did not receive one at the time of my SCAD heart attack. Why?
I experienced a lot of on-going chest pain for quite some time after my SCAD. Why does this happen and is this normal? What other symptoms can I expect to experience as part of my recovery? How do I know if my dissection has healed and can it happen again?
What medications do most patients with SCAD take? How long will I need to take the medications? What should I do if I have side effects?
Should I participate in cardiac rehabilitation? How might CR help me understand and manage any new limits I need to consider?
I have experienced a lot of stress and anxiety since having a SCAD. Where can I go for help with this?
Is it safe for me to breastfeed, get pregnant again and have more children? Are contraceptives or HRT therapies safe for me now? My periods have been much worse since my SCAD, why is that?
What does the road ahead look like for patients with SCAD?
How frequently should I be seeing a cardiologist or my family doctor? When can I return to work? Will I be able to do my job the way I did before?
Additional resources
- Spontaneous Coronary Artery Dissection : A Guide for Patients and Caregivers (PDF)
- Vancouver General Hospital: Offers the first cardiac rehabilitation program specifically for women with a diagnosis of SCAD.
- SCAD Alliance: A non-profit organization dedicated to raising awareness, supporting research, and providing education and resources for those affected by SCAD. Their website includes a list of support groups to help patients and their families connect, share experiences, and find encouragement.
- Sunnybrook Hospital: A patient-friendly guide that explains what SCAD is, its causes, symptoms, diagnosis, and treatment, as well as recovery tips and lifestyle considerations.
- The Mayo Clinic: A detailed overview of SCAD, including symptoms, possible causes, risk factors, complications, and when to seek medical help.
- The Cleveland Clinic: Information on SCAD symptoms, causes, diagnosis, treatment options, and strategies for recovery and prevention.
- The Heart and Stroke Foundation: An accessible resource in English and French about SCAD, its impact on the heart, risk factors, and how to live well after diagnosis.