Description
What is mitral regurgitation?
Mitral regurgitation (MR) is a heart problem that happens when the mitral valve doesn’t close the way it should. The mitral valve is one of four valves in the heart that make sure blood flows in the right direction.
Typically, blood moves through the heart in one continuous path.
It enters the right side of the heart and then goes to the lungs to pick up oxygen. From the lungs, it travels to the left side of the heart. There, it passes through the mitral valve into the lower left chamber before being pumped out to the rest of the body.
When someone has MR, the mitral valve leaks and some blood flows backward. This can make the heart work harder and weaken over time. If MR worsens, it can cause symptoms such as tiredness, shortness of breath, and trouble doing typical or routine daily activities.
What is mitral valve transcatheter edge-to-edge repair (M-TEER)?
For many people with MR, medications may not be enough. In some cases, traditional surgery is not possible — especially for patients with heart failure or those at high risk for open-heart surgery. For these patients, a less invasive option called transcatheter mitral valve repair (TMVr), also known as transcatheter edge-to-edge repair (TEER) using Abbott’s MitraClip™ therapy or Edwards’ PASCAL™ therapy, may be available.
This procedure is designed to reduce backward leakage in the mitral valve so blood flows properly through the heart. It is performed without open-heart surgery. Instead, doctors make a small incision in the leg and guide a thin tube (catheter) through a large vein up to the heart. A tiny implant is then attached to the leaflets of the mitral valve, helping the valve close completely and restoring blood flow.
The procedure usually lasts one to three hours, and most patients can go home the next day. Many people notice improvement in their symptoms — such as less shortness of breath and more energy — soon after the procedure, leading to a better quality of life.
What is tricuspid regurgitation?
Tricuspid regurgitation (TR) is a heart problem that happens when the tricuspid valve doesn’t close the way it should. The tricuspid valve is one of the four valves in the heart. It controls blood flow on the right side of the heart.
Typically, blood flows from the body into the upper right chamber of the heart. It then passes through the tricuspid valve into the lower right chamber. From there, the blood goes to the lungs to pick up oxygen before returning to the left side of the heart where it is pumped out to the body.
When someone has TR, the tricuspid valve leaks and some blood flows backward into the upper right chamber. This can make the heart work harder and lead to symptoms such as swelling in the legs or belly, tiredness, and shortness of breath. Over time, TR can affect how well the heart pumps blood through the body. If TR worsens, it can cause symptoms such as shortness of breath, peripheral edema (swelling in the legs, angles and feet), ascites (buildup of fluid in the abdomen), fatigue, and declining exercise capacity.
What is tricuspid transcatheter edge-to-edge repair (T-TEER)?
Some people with TR, or a leaky tricuspid valve, do not get better with medicine. For many, open-heart surgery is too risky because of other heart problems or health issues. In these cases, a less invasive treatment called TriClip™ therapy (also called transcatheter tricuspid valve repair or TEER) may be an option.
This procedure helps fix the leaky tricuspid valve so blood can flow properly through the right side of the heart. Instead of open-heart surgery, doctors make a small cut in the leg. A thin tube (catheter) is placed in a large vein and guided to the heart. Through this tube, the doctor attaches a small device called the TriClip™ to the tricuspid valve. The clip helps the valve close more tightly and reduces the leak.
The procedure usually takes two to three hours. Most patients can go home the next day. Many people feel better quickly. They may have less swelling, breathe easier, and find it easier to do typical or routine daily activities.
Patient instructions
Patient evaluation for TEER therapy
Before deciding if TEER is right for you, your care team will go through several steps.
- Referral: Your cardiologist refers you to the heart team for evaluation.
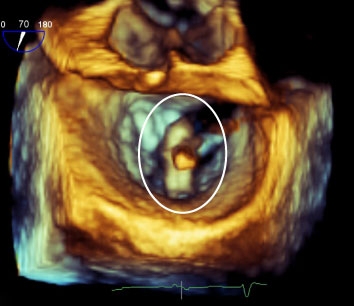
- Heart ultrasound: You will need recent transthoracic echocardiogram (TTE) images and reports. A standard echocardiogram is an imaging technology that uses ultrasound to create images of your heart. It is a diagnostic test used to examine the heart and its blood supply, determine how large the heart is, how well it contracts, and how the valves function.
- Detailed heart ultrasound: You will also need recent transesophageal echocardiogram (TEE) images and reports for a closer look at your valve. A TEE uses ultrasound to create images of your heart with a specialized probe, which is inserted into the esophagus. This test provides information about how large the heart is, how well it contracts, and how the valves function.
- Heart team review: The doctors review your images together at a weekly meeting. Cardiologists, interventional cardiologists, cardiac surgeons, anesthetists specializing in the TEER procedures, echocardiographers, nurses, and research staff are present.
- Decision: The heart team decides the best option for you. This may include:
- Continued observation and follow-up
- A TEER procedure
- Open-heart surgery
- Participation in a research study
- Or, if no treatment is possible, focusing on symptom care
Next steps if TEER is recommended
- Meet with the interventional cardiologist: Talk with the doctor who will perform the procedure. They will review the benefits and risks of the procedure, and explain why you are or are not a candidate for this type of intervention.
- Pre-Admission Unit appointment: Meet with the nursing team and anesthesia team. This visit includes:
- Reviewing your medications and medical history
- Bloodwork, ECG, and a chest X-ray
- Further pre-procedure instructions
- Phone call to confirm: You will receive a phone call to confirm the date and time of your procedure.
Post procedure
Most patients come to the Recovery Unit already breathing on their own. If you still need a breathing tube, a nurse will remove it as soon as you are awake and can follow directions. A nurse will stay with you until you are breathing comfortably.
For the first two to four hours after your procedure, the nurse will remind you to keep your legs straight. This helps prevent bleeding from the small cuts in your groin where the tubes were placed.
You will stay in the Recovery Unit overnight or longer if needed. Your nurse will check on you often and make sure you are comfortable. Tell the nurse right away if you feel pain.
As you get stronger, you will slowly increase your activity. First, you will sit up in bed. Then, you will sit in a chair. Later, you will walk with help.
That night, you may start with clear liquids (like water, broth, or juice). By the next day, you should be able to eat your regular diet.
Nurses will remove most of the special monitors the next morning. Once you are stable, you will be ready to leave the Recovery Unit.
The day after your procedure, you will have:
- An echocardiogram (TTE) to check how the clip is working
- Blood tests
- A chest X-ray
- An ECG (heart tracing)
A nurse will check the spot in your groin where the tube was placed and show you what to watch for at home. They will remove the stitches in the morning. A small bruise or soft lump is typical, and bruising may move down your leg.
Call your nurse or doctor if you notice:
- A lump that is getting bigger, or redness and warmth that does not go away
- Yellow fluid (pus) coming from the site
- Numbness in your leg that is getting worse
- Severe pain at the site
Additional info
For more information, please contact the Structural Heart Coordinator at 613-696-7000.
Patient Resources
Referring doctor
Please complete the patient registry form with accompanying documentation and fax it to UOHI Triage: 613-696-7144.
Please also send patient's TTE and TEE images to the Triage Office.